Turning Back the Clock: Our Protective Outer Layer
Throughout our lives, our skin goes through a lot. We get sunburns, we skin our knees, we bleed, we scar, and we do it again. Our skin is our largest organ and, in many ways, serves as our protector. Beyond acting as a protective barrier between us and our environment, our skin regulates our body temperature, provides immune protection against harmful microbes and blocks out harmful sunlight in ways that benefit the whole body. And when skin is injured, blood brings healing substances to the site to promote healing as the body awaits new, replacement skin cells.
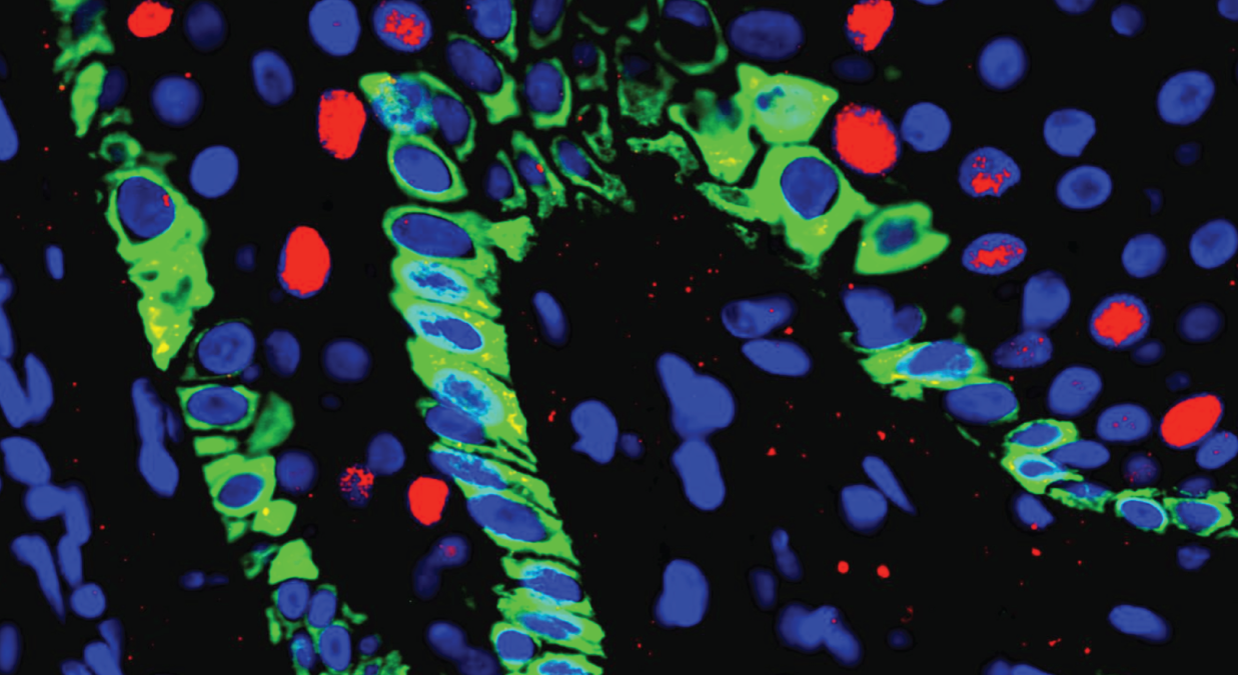
Regardless of scrapes and scratches, skin cells are constantly renewing themselves throughout our lives — a process reliant on skin stem cells. These skin stem cells turn over slowly, keeping our skin healthy and young. But as we age, these skin stem cells either numerically or functionally deplete, our skin thins, and we are consequentially at higher risk for developing ulcers. The older the skin, the harder it is to heal these ulcers, meaning they can become chronic, open wounds that impact lifestyle and invite infection.
But what if we could activate a skin stem cell to be more responsive to injury? To get an 80-year-old’s skin to function like a 30-year-old’s skin? Could we reverse skin stem cell age-related deterioration and improve their turnover? What if we could do so in a way that healed wounds regeneratively, without any scarring? With these questions in mind, a collaborative team of researchers from the Mass General Brigham, Boston Children’s Hospital, and four additional Harvard institutions set off to study these powerful cells.
Advancing Skin Stem Cell Research
“As a dermatopathologist, I’m always fascinated by how the skin is potentially a model and a proxy for what is going on in other vital organs,” said George Murphy, MD, director of the Brigham’s Program in Dermatopathology and professor of pathology at Harvard Medical School. “Skin is accessible to study in a way that internal organs are not. The idea that physiologic stem cells may be involved in so many seemingly divergent pathologies — whether they be cancer, skin dermatitis, wound healing or chronologic aging — makes it such an exciting area to discover the secrets of stem cell biology.”
Markus Frank, MD, associate professor of pediatrics and dermatology at Harvard Medical School and research scientist at Boston Children’s Hospital’s Department of Medicine and the Brigham’s Department of Dermatology, who co-leads the Harvard Stem Cell Institute Skin Program along with Murphy, added: “The possibility of reversing age-related skin stem cell dysfunction or depletion through in vivo stem cell reprogramming or through stem cell transplantation holds great promise for injured or aged skin regeneration and/or rejuvenation.”
Recently, Murphy, Frank and additional colleagues from the Brigham, Boston Children’s Hospital, Mass General, Harvard Stem Cell Institute, Harvard School of Public Health, Harvard Medical School and the Schepens Eye Research Institute of Mass Eye and Ear have begun a collaborative program researching skin stem cells. The team was awarded $10.89 million by the National Institute for Aging for their project entitled “Multicomponent Therapy for Age-related Skin Stem Cell Deficiency.” This funding will help accelerate the pre-existing program, which had been steadily progressing over the last three years in collaboration with the Harvard Stem Cell Institute Skin Program.
Before assuming their roles as leaders and co-principal investigators of this novel skin stem cell program project award, both Murphy and Frank had long explored similar research topics. Murphy started working with the potential for skin to regenerate after injury in the 1980s when working with Dennis Orgill, MD, PhD, at BWH and Ioannis Yannas, PhD, at MIT, and revisited the subject with more intention in 2004, when Frank, too, following his and BWH geneticist Dr. Natasha Frank’s joint discovery of the stem cell-associated ABCB5 gene in 2003, began focusing more time on skin stem cells. The shared interest led to a Nature cover featuring a co-authored landmark study from the Franks and Murphy labs, and colleagues including then post-doctoral fellow, Tobias Schatton, which marked the first identification and targeting of stem cells responsible for malignant melanoma.
In collaboration with their many colleagues, Murphy and Frank have set off to ask critical questions about skin stem cells, with the ever-present goal of improving patient care. The grant will fund a two-part goal: to map metabolomic, epigenetic and cell receptor stem pathways involved in age-related defective wound healing; and to develop novel stem cell-directed multicomponent combinatorial therapies. The interdisciplinary team will pursue these goals over the next five years.
While the program primarily is working to gain insight into skin stem cell biology, it may also inform the study of cancer, aging and stem cells in organs other than the skin. Ultimately, skin stem cells are tissue-based stem cells, which means studying them may lead to a better understanding of other bodily tissues and pathologies. Ideally, this program will enhance scientific interest in physiologic organ-resident stem cells, in addition to complementary work by others focused on pluripotent and embryonic stem cells.
The program also offers a model for interdisciplinary collaboration. When asked about the collaborative aspect of the program, Murphy said, “This program unites Harvard institutions and their scientists, combining training, expertise, and resources from a multitude of sophisticated disciplines. The rising popularity of the interdisciplinary team-science approach to medical problems is for good reason — we simply work more efficiently and more creatively when we do it together.”
The seven-way collaboration unites epigenetics, cell biology, metabolomics, bioinformatics and immunopathology. Such diversity in training allows for diversity in solutions, as well as new connections between researchers.
“We are on the cusp of a perfect storm where highly integrated team science and technology can now take on this problem in a completely novel way,” said Frank. “We can create new approaches that target and reverse age-related stem cell depletion in order to not only heal recalcitrant skin ulcers, but to provide insights into how regenerative healing may be achieved in skin, and potentially even beyond.”
Co-investigators of the program project grant include:
- Natasha Frank, MD, BWH Division of Genetics
- Ya-Chieh Hsu, PhD, Harvard Department of Stem Cell and Regenerative Biology
- Shannan Ho Sui, PhD, the Harvard T.H. Chan School of Public Health Bioinformatics Core
- Bruce Ksander, PhD, the Schepens Eye Research Institute of Massachusetts Eye and Ear
- Christine Lian, MD, BWH Department of Pathology
- Anna Mandinova, MD, PhD, MGH Cutaneous Biology Research Center
- David Sinclair, PhD, the Paul F. Glenn Center for Biology of Aging Research at Harvard Medical School
- Seung-Schik Yoo, PhD, BWH Department of Radiology